The Clinical and Therapeutic Implications of Meal Replacements: Sustained Weight Loss for Improved Liver Health and Diabetes Remission
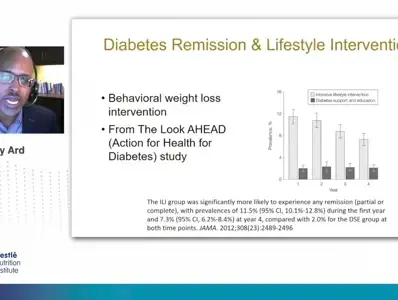
The epidemic of obesity and type 2 diabetes have become a global public health issue. The World Health Organization (WHO) estimates there are over 650 billion adults worldwide affected by overweight and obesity, and the International Diabetes Federation reports approximately 537 million adults are living with type 2 diabetes. For many, overweight and obesity is the result of a combination of a high-caloric and high fat diet, little to no physical activity, and a genetic predisposition. Obesity increases a person’s risk of developing type 2 diabetes as well as other concomitant conditions like hypertension, dyslipidemia, and nonalcoholic fatty liver disease. To reduce the risk of developing type 2 diabetes and to improve patient outcomes, clinical guidelines recommend nutrition intervention and a reduction of 5-10% in body weight, which can be achieved using either or both nonpharmacological interventions, such as a low energy diet, or pharmacological interventions. In this symposium, Dr. Jamy Ard reviews the nutritional approaches for the management of type 2 diabetes and the clinical application of using meal replacements as a very-low calorie diet (VLCD) for improved cardiometabolic parameters and to achieve diabetes remission. Dr. Ard also examines the clinical evidence on the effectiveness and long-term implications of using meal replacements as a very low-calorie diet to achieve improved glucose control and diabetes remission. Dr. Wajahat Mehal discusses the pathophysiology of non-alcoholic fatty liver disease (NAFLD), the relationship between nutritional approaches and patient outcomes for the management of non-alcoholic fatty liver disease, and the clinical evidence on using meal replacements as a very low-calorie diet for sustained weight loss and improved liver health.
If you liked this post you may also like