Breastfeeding & Cow Milk Protein Allergy: What You Need to Know
Cow milk protein allergy (CMPA) is the most common cause of food allergies in infants and young children less than 3 years old1 It presents multiple ways and is the result of an immunologic response to cow milk proteins, which may be IgE or non-IgE-mediated.
Symptoms may occur in infants during their first few months of life, usually days or even weeks after a cow milk-based formula is given. Symptoms may be immediate or delayed, may be mild or life-threatening.
One should keep in mind though, that CMPA may also present in infants who are exclusively breastfed. This takes place if cow milk protein from the mother’s diet is delivered in the breast milk in sufficient amounts.
Unfortunately, there isn’t just one set of symptoms that are specific to cow milk protein allergy. Table 1 summarizes the most frequent presentations.2 It is crucial to look at timing and the pattern of the symptoms. Many of those with CMPA have symptoms in at least two of the following organ systems: gastrointestinal (50-60%), cutaneous (50-60%) and respiratory tract (20-30%). The symptoms are very common in otherwise well infants or those with other diagnoses, so clinical judgment is required. 3,4
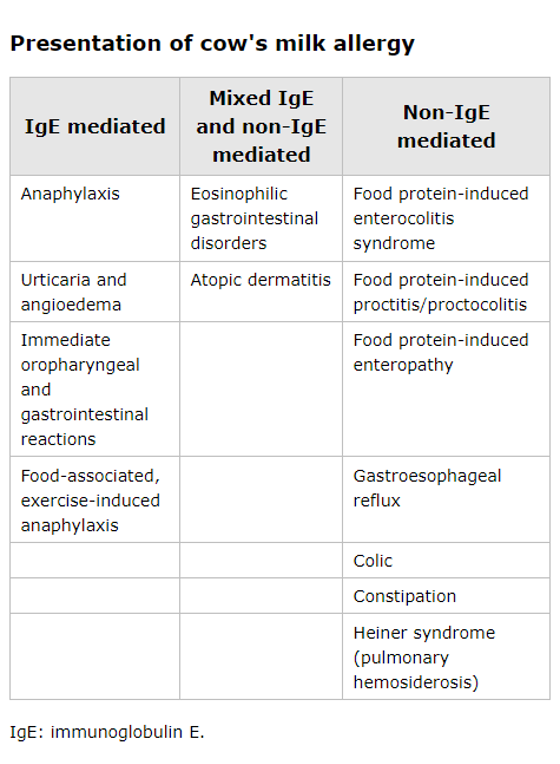
Adapted from reference 2
AIn assessing infants with suspected cow milk allergy, it is important to have an allergy-focused clinical history. This is the cornerstone of diagnosis. One should ask about a family history of atopic disease among parents or siblings. Symptoms of suspected cow milk allergy plus a family history of allergic disease make CMPA a more likely diagnosis. It is also important to ask the source of cow milk protein and how much is being ingested. If the infant is exclusively breastfed, then the cow milk protein may be coming from maternal ingestion passing through breastmilk. If the infant is being given mixed feeds or as purely formula-fed infants, obtain details of reproducibility upon repeated ingestion.5
Diagnosing CMA is based on the history and lab tests, if available (diagnostic tests for non-IgE-mediated manifestations of CMA are limited). The gold standard for diagnosis is a clinician-supervised, double-blind, placebo-controlled oral food challenge, although an open challenge is the established route taken. Determining the level of cow's milk-specific IgE may be helpful in clinching the diagnosis of IgE-mediated CMA and may eliminate the need for oral food challenges.6
Depending on the clinical presentation, available tests include in vitro immunoassays for specific IgE to cow milk protein, skin prick testing and oral food challenges which are requested and performed by board-certified allergists.2
When the history and testing are not conclusive, the diagnostic procedure may include elimination of the suspected food for two to eight weeks.7 If the probability is higher, this is followed by a challenge. Reintroduction may be presented if the probability is lower.
BREASTFEEDING & COW MILK PROTEIN ALLERGY
The most straightforward approach in managing any food allergy is complete avoidance of the culprit food. CM is a ubiquitous food in many cultures and diets and is an important source of fat and protein in early childhood, so eliminating CM from the diet can be complicated and can result in nutritional as well as quality-of-life concerns.2
In this particular article, we will address the management of CMPA in exclusively breastfed infants. We all know that breast feeding is the gold standard in infant nutrition and is recommended exclusively for the first 4 months of life at least.
Breastfeeding is recommended in the primary prevention of allergy, but in situations where breast-fed infants are proven to have CMPA, allergen avoidance is advised. Evidence tells us that food proteins, not just from cow’s milk, but from other foods may result in reactions even in exclusive breastfeeding in sensitized infants. These causal food include eggs, peanut and wheat which are excreted in the mother’s breast milk.4
Because of the many benefits of breast feeding to the infant and the mother, clinicians should still advise mothers to continue breast feeding but avoid the causal foods in their own diet.
Guidelines and recommendations regarding cow milk protein allergy have been widely published by different societies & groups to help physicians maneuver through the challenges of management.
One such document that may prove to be helpful is the International Milk Allergy in Primary Care (iMAP) guideline, released as a practical guide, in simple algorithms, for managing more common presentations of CMPA.5,8 This is an iteration of the 2013 MAP published for the benefit of UK clinicians that eventually gained international popularity.
The algorithm (Figure 1) included here is adapted from the iMAP as well as the review article by Vandenplas in 2007 and may prove helpful for the “first contact clinicians”.

Majority of infants will outgrow CMPA, but as to when, there is not specific time. This is why monitoring for resolution is important. It includes looking at regular testing for sensitization (in vitro tests or skin prick tests), checking for accidental exposures and reactions and even oral food challenges.
SUMMARY
Cow milk protein allergy is the most common food allergy in children. Manifestations include IgE-mediated reactions (urticaria, anaphylaxis), non-IgE reactions (delayed gastrointestinal manifestations) or mixed reactions (atopic dermatitis).
Diagnosis is based on proper history-taking and laboratory tests (skin prick tests, in vitro test oral challenges).
Management includes advice regarding avoidance and replacement. Breastfeeding is highly encouraged with the proper advice for mothers to address nutritional or even quality of life concerns. It is also highly suggested to refer to an allergist for co-management.
REFERENCES
1 Rona RJ, Keil T, Summers C, Gislason D, Zuidmeer L, Sodergren E, Sigurdardottir ST, Lindner T, Goldhahn K, Dahlstrom J, McBride D, Madsen C. The prevalence of food allergy: a meta-analysis. J Allergy Clin Immunol. 2007 Sep;120(3):638-46.
2 Jarvinen-Seppo, KM, (2021). Milk allergy: Clinical features and diagnosis. In Sicherer, SH & TePas, E (Ed.), UpToDate. Retrieved May 24, 2022, https://www.uptodate.com/contents/milk-allergy-clinical-features-and-diagnosis.
3 Host A. Frequency of cow’s milk allergy in childhood. Ann Allergy Immunol 2002;89(Suppl 1):33–7.
4 Vandenplas Y, Koletzko S, Isolauri E, Hill D, Oranje AP, Brueton M, Staiano A, Dupont C. Guidelines for the diagnosis and management of cow's milk protein allergy in infants. Arch Dis Child. 2007 Oct;92(10):902-8.
5 Venter C, Brown T, Meyer R, Walsh J, Shah N, Nowak-Węgrzyn A, Chen TX, Fleischer DM, Heine RG, Levin M, Vieira MC, Fox AT. Better recognition, diagnosis and management of non-IgE-mediated cow's milk allergy in infancy: iMAP-an international interpretation of the MAP (Milk Allergy in Primary Care) guideline. Clin Transl Allergy. 2017 Aug 23;7:26.
6 Fiocchi A, Brozek J, Schünemann H, Bahna SL, von Berg A, Beyer K, Bozzola M, Bradsher J, Compalati E, Ebisawa M, Guzmán MA, Li H, Heine RG, Keith P, Lack G, Landi M, Martelli A, Rancé F, Sampson H, Stein A, Terracciano L, Vieths S; World Allergy Organization (WAO) Special Committee on Food Allergy. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow's Milk Allergy (DRACMA) Guidelines. Pediatr Allergy Immunol. 2010 Jul;21 Suppl 21:1-125.
7 NIAID-Sponsored Expert Panel, Boyce JA, Assa'ad A, Burks AW, Jones SM, Sampson HA, Wood RA, Plaut M, Cooper SF, Fenton MJ, Arshad SH, Bahna SL, Beck LA, Byrd-Bredbenner C, Camargo CA Jr, Eichenfield L, Furuta GT, Hanifin JM, Jones C, Kraft M, Levy BD, Lieberman P, Luccioli S, McCall KM, Schneider LC, Simon RA, Simons FE, Teach SJ, Yawn BP, Schwaninger JM. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010 Dec;126(6 Suppl):S1-58.
8 Fox A, Brown T, Walsh J, Venter C, Meyer R, Nowak-Wegrzyn A, Levin M, Spawls H, Beatson J, Lovis MT, Vieira MC, Fleischer D. An update to the Milk Allergy in Primary Care guideline. Clin Transl Allergy. 2019 Aug 12;9:40.
If you liked this post you may also like