Carbs clock: Timing of meal as well as composition influences glycemic response – first-of-a-kind study
Researchers have revealed that the timing of carbohydrate-rich meals can significantly worsen glucose homeostasis – on top of the independent glycemic index of the food – potentially revealing ways to minimise the risk of type-2 diabetes.
It has long been known that the glycemic index or load (GI/GL) of a meal affects the glycemic response of the subsequent meal.
However, this is the first study to assess the timing of the meal and GI variations on the subsequent meal effect concurrently.
Researchers from Singapore and Switzerland reported that consuming a carbohydrate-rich meal during dinner compared to breakfast resulted in a significant spike in glucose levels, which was then carried to the following meal.
Published in the journal BMJ Open Diabetes Research & Care, first author, Dr Sumanto Haldar, from Singapore’s Clinical Nutrition Research Centre told NutraIngredients-Asia: “This is the first study in the world, which simultaneously looked at the effects of both timing and GI on various markers of postprandial glycemic control, not only after the meal itself but also after the subsequent meals (i.e., second meal effect).”
Postprandial glucose (PPG) homeostasis is an important determinant for the risk of chronic diseases, in particular type 2 diabetes and cardiovascular diseases.
Conducted on an Asian population, this study is crucial as Asians have a greater predisposition to develop type 2 diabetes and prediabetes as compared with the Western Caucasian populations.
This study was jointly funded by the Singapore Institute for Clinical Sciences, Agency for Science, Technology and Research (A*STAR), Singapore and Nestle.
Study design
In this randomised controlled trial, 34 healthy Chinese subjects aged 50 to 70 years were recruited in Singapore.
Each subject completed four separate intervention sessions (test meals) for the study, in a random order, consisting of high-GI breakfast (Hi-Br), low-GI breakfast (Lo-Br), high-GI dinner (Hi-Di) and low-GI dinner (Lo-Di).
All test meals contained approximately 75g available carbohydrates, made from either high GI rice (GI:92) or low GI rice (GI:55), flavored with a small amount of chicken seasoning and 20g green leafy vegetables to ensure palatability.
Following the tests, subjects were also given a standard meal to consume at the next meal time.
Blood samples were collected at baseline, 15, 30, 45, 60, 90, 120 during both test meals and standard meals.
Postprandial metabolic response was calculated using the incremental areas under the curve (iAUCs).
Findings
As expected, the high GI test meals resulted in significantly greater iAUCs of PPG (p<0.0001) compared to lower GI test meals, irrespective of mealtime.
However, the iAUCs of PPG (p<0.0001) following dinner test meals were greater than breakfast, irrespective of the GI content of the meals.
Researchers observed that glycemic control was worse in the later part of the day and advised “to focus on carbohydrate quality and quantity of the evening meals, particularly in preventing future risk of type 2 diabetes and related cardio-metabolic diseases.”
The implications of these findings are especially relevant in Asia, where carbohydrate-rich, high GI meals in the form of starches and grains are often consumed late during the day due to cultural practices.
Researchers cited a recent study where healthy adults in India consumed about 32% of their daily calories between 7 to 10pm, with the median dinnertime being after 10 pm.
They wrote: “This observation is particularly important since majority of the epidemiological studies investigating associations between GI/GL of the diet and disease risk generally ignore considerations on assessing the timing of the consumption in addition to calculating the mean daily GI/GL contents of the foods.”
“An individual habitually consuming proportionately greater GL during dinner may have an overall worse glycemic status than someone else who habitually consumes greater GL for breakfast, even though their mean daily GL may be similar.”
Limitation and recommendations
As the study was conducted on healthy subjects, researchers said their findings may not be applicable to type 2 diabetics, explaining that insulin sensitivity may differ in the diabetic group.
In addition, due to the acute design of the study, long-term validity of its findings would need to be confirmed.
Dr. Haldar told us: “The next steps for our team will be to undertake longer term dietary intervention trials, with specific dietary components such as low GI, or rich in phytonutrients, suited for specific times during the day (i.e., chrono-nutrition), in order to improve the risk of cardio-metabolic diseases such as diabetes, CVD etc. We are in the process of planning such studies.”
Source: BMJ Open Diabetes Research & Care
doi:10.1136/bmjdrc-2019-001099
“High or low glycemic index (GI) meals at dinner results in greater postprandial glycemia compared with breakfast: a randomized controlled trial”
Authors: Sumanto Haldar, et al
If you liked this post you may also like
Food, planet and health: A complex equation to solve

Eating better: Enhancing health, sustainability, and food security
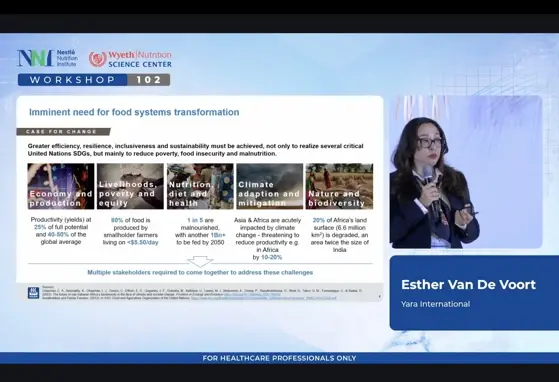
Digital Agriculture: New frontiers for the food system

Round Table: Healthy growth within a healthy planet