The early protein hypothesis: excessive protein intake in early infancy

As the obesity epidemic marches on across the globe, we have now reached a point where as many as 200 million school-age children are suffering from weight-related problems.1 Even more worrying, the situation is becoming worse and worse, with 1 in 2 infants destined to become obese in later life if current trends continue. This surge in obesity is not just a problem of appearances. Obesity is associated with a number of serious health problems – including heart disease, type 2 diabetes and an increased risk of cancer – and the financial costs to society are enormous. It’s easy to see why the World Health Organization describes obesity and obesity-related diseases as one of the most serious public health challenges of the 21st Century, and why obesity prevention is such a pressing cause.
Key risk factors in early infancy associated with later obesity
We are not all born equal when it comes to obesity. Infants are more likely to have weight problems later in life if their mother is overweight or obese, if they weigh more than 4 kilograms at birth, if they gain weight rapidly in early life, and if they are not breastfed. Given that a huge number of women of child-bearing age are overweight or choose not to breastfeed, the number of infants at higher risk of being overweight or obese later in life is growing.
It is not immediately obvious why breastfeeding protects infants against obesity in later life. One key factor appears to lie in its protein content. According to the so-called ‘early protein hypothesis’, a high protein intake in early infancy is linked with a higher number of fat cells as the child grows. It is thought that a high protein intake increases the release of insulin (the hormone that controls the metabolism of carbohydrates and fats) and IGF-1 (a hormone produced mainly by the liver that behaves in a similar way to insulin). Studies carried out by researchers for the Childhood Obesity Project (CHOP) in Europe and other groups support the early protein hypothesis, confirming that high protein intakes in infancy cause faster weight gain and higher body mass index (BMI) in the first years of life.2
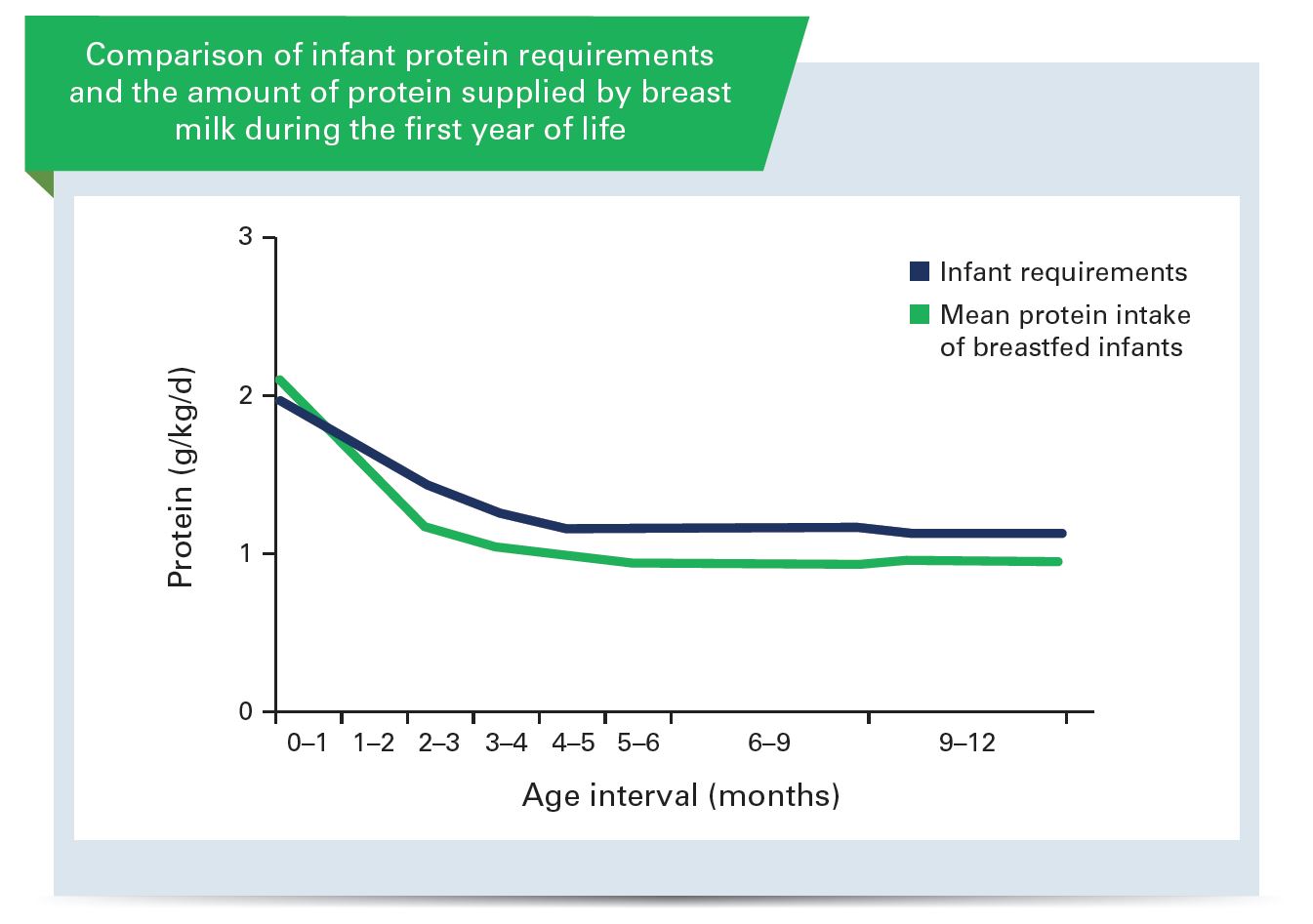
Breast milk – a naturally balanced protein supply
So how much protein does breast milk contain? Interestingly enough, it’s almost exactly the amount that an infant needs as it grows. Plotting a graph of mean protein intake of breastfed infants up to 12 months of age shows that the protein provided by breast milk always matches the infant’s protein requirements very closely. As the speed at which the infant grows declines, so does the protein content of breast milk.
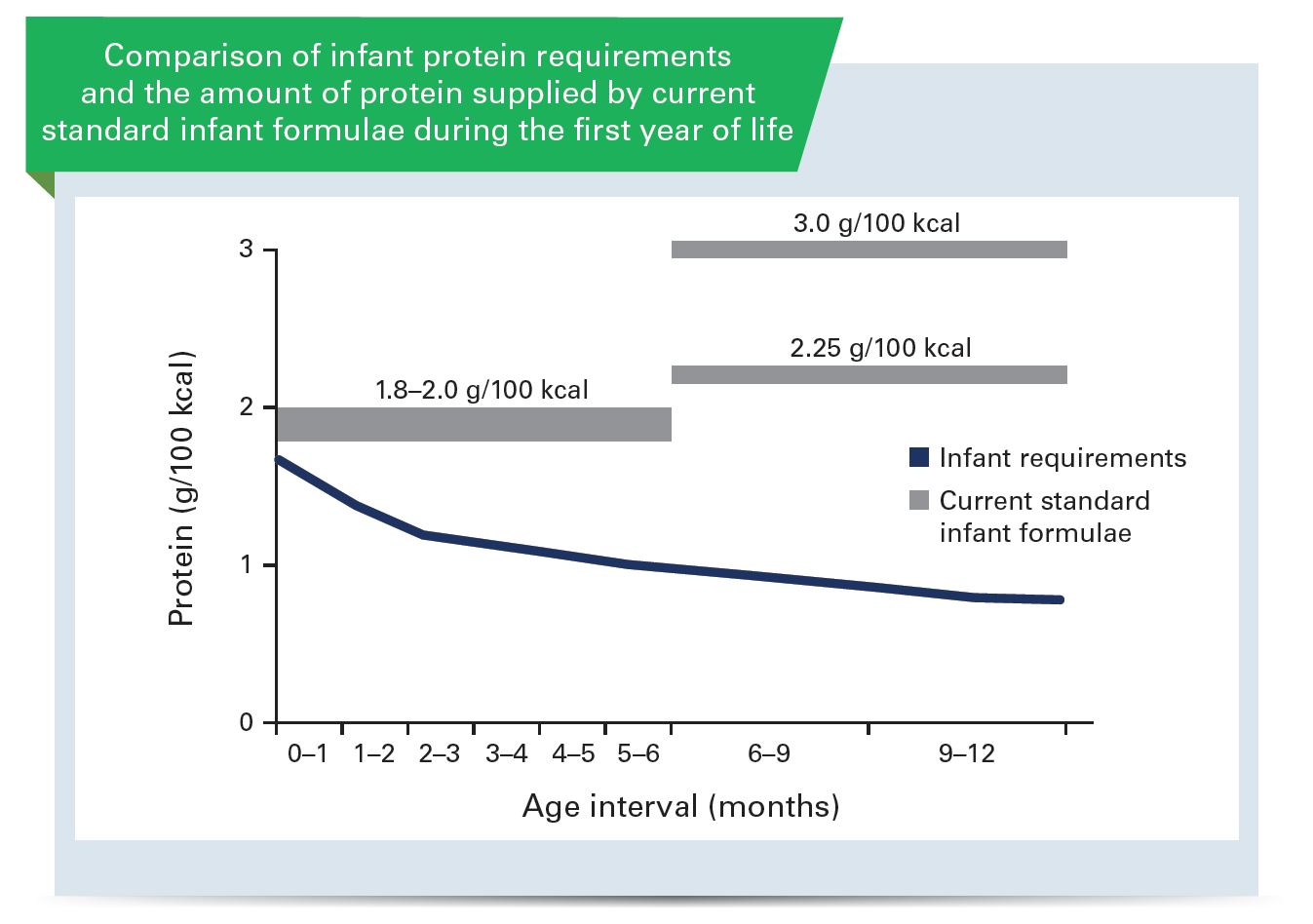
A standard infant feeding formula contains around 2 grams of protein per 100 calories, and this is typically given for the first 6 months of life. After the first 1–2 months, however, this is already well above the amount of protein that the child really needs. So what do we do at 6 months of age? Rather than giving formula-fed infants less protein, many older-infant formulas actually have higher protein contents – as much as 3 grams per 100 calories. This means that, unlike those who are breastfed, formula-fed infants receive excessive amounts of protein in the critical first year of life.
Does less protein equal fewer problems?
A recent study carried out in Chile looked at the potential benefits of replacing standard feeding formula (2.7 grams per 100 calories) with a lower-protein alternative (1.65 grams per 100 calories) at 3 months in children born to overweight or obese mothers – and therefore already at elevated risk of becoming obese in later life. Breastfed infants were also included in the study, to act as a control group.3
What the study showed was that infants fed the lower-protein formula from 3 months of age gained weight at a similar rate to breastfed infants. When the groups were compared at 2 years, infants fed the standard formula weighed an average of 518 grams more than infants fed the lower-protein formula. A similar benefit at 2 years was seen for BMI. Infants who received the lower-protein formula had a BMI close to that of breastfed infants. Other growth measurements, such as head circumference and body length, were perfectly normal in infants fed the low-protein formula.
Perhaps most interestingly, the benefits of the lower-protein formula were maintained for 1 year after feeding with the lower-protein formula stopped, suggesting that use of this formula in early infancy may have a long-term effect on healthy weight development.
Key references:
1. International Obesity Taskforce. The global epidemic. http://www.iaso.org/iotf/obesity/obesitytheglobalepidemic/
2. Koletzko B, Broekaert I, Demmelmair H, et al. Protein intake in the first year of life: a risk factor for later obesity? The E.U. childhood obesity project. Adv Exp Med Biol 2005;569:69–79.
3. Martin FP, Moco S, Montoliu I, et al. Impact of breast-feeding and high- and low-protein formula on the metabolism and growth of infants from overweight and obese mothers. Pediatr Res 2013 Dec 27. doi: 10.1038/pr.2013.250 [Epub ahead of print]
To watch the full presentation, click here
See our other experts opinion

Antibiotics Early in Life Alter Colonization and Predisposes to Obesity
Microbiota and Obesity

Human Milk Oligosaccharides Functional Outcomes
Human Milk Oligosaccharides – Compositional Analysis and Metabolism in Infants